MANAGEMENT TIPS FOR TYPE 1 DIABETES
Diabetes, also known as diabetes mellitus is a condition where the blood sugar levels are higher than normal. There are two major categories of diabetes, type 1 also known as juvenile or early-onset insulin-dependent diabetes and type 2, non-insulin-dependent diabetes.
Type 1 diabetes usually develops quite quickly over a few days or weeks. It is due to an autoimmune condition whereby the body starts producing antibodies against itself, more specifically against the beta cells in the pancreas which are involved in insulin production. Only in rare conditions is it due to other causes such as surgical removal of the pancreas or severe inflammation of the pancreas.
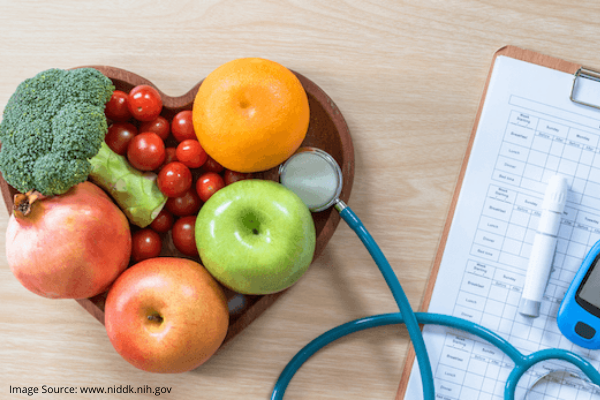
Insulin is an essential hormone necessary for controlling blood glucose levels; if the blood glucose levels remain too high over period of time, irreversible damage starts to set in among the various organs and lead to certain death. Treatment is by the regular use of insulin injections and by following a healthy diet that’s controlled in carbohydrates.
Type 1 diabetes can set in from early childhood, sometimes even below the age of 5 years; it accounts for about 90% of diabetes cases among those below 25 years of age. About 15% of diabetic children also have a first-degree relative with diabetes too. Children with diabetic fathers have greater chances of developing diabetes as compared to children with diabetic mothers.
Managing diabetes in youngsters, especially in children as young as 5 years or less is a major challenge that parents get to face every day. Maintaining blood glucose levels in the normal range requires a constant balancing act among various parameters such as diet, exercise, stress, general health, medications, etc. Before a management plan can be formulated, a general assessment of the health and lifestyle of the patient needs to be taken into consideration.
Treatment basically involves lifelong insulin replacement injections or the use of an insulin pump. Blood glucose levels will have to be monitored daily, sometimes up to 6 times a day. Basically the patient gets to decide how much insulin to take depending on the sugar level – close collaboration with the doctor and understanding the limits of insulin use are essential here. The diet needs to be monitored carefully too with carbohydrates spread out over the day coupled with regular physical activity or exercise. Aside from lowering the risk of cardiac diseases, exercise also promotes the optimal use of the insulin.
The patient would also need to go for regular check-ups and routine screenings for eyes, heart, kidneys, blood vessels and nerve diseases. Abstaining from smoking and alcohol also helps diabetic people avoid complications from periods of low blood sugar levels.
Blood sugar levels are also easier to control and maintain if there is a daily routine for mealtimes, specific meal plans and proper exercises.
However, once your sugar levels reach near the normal limits, you will still need to keep taking minimal doses of insulin to decrease the stress on the pancreas.














