WORLD HEPATITIS DAY
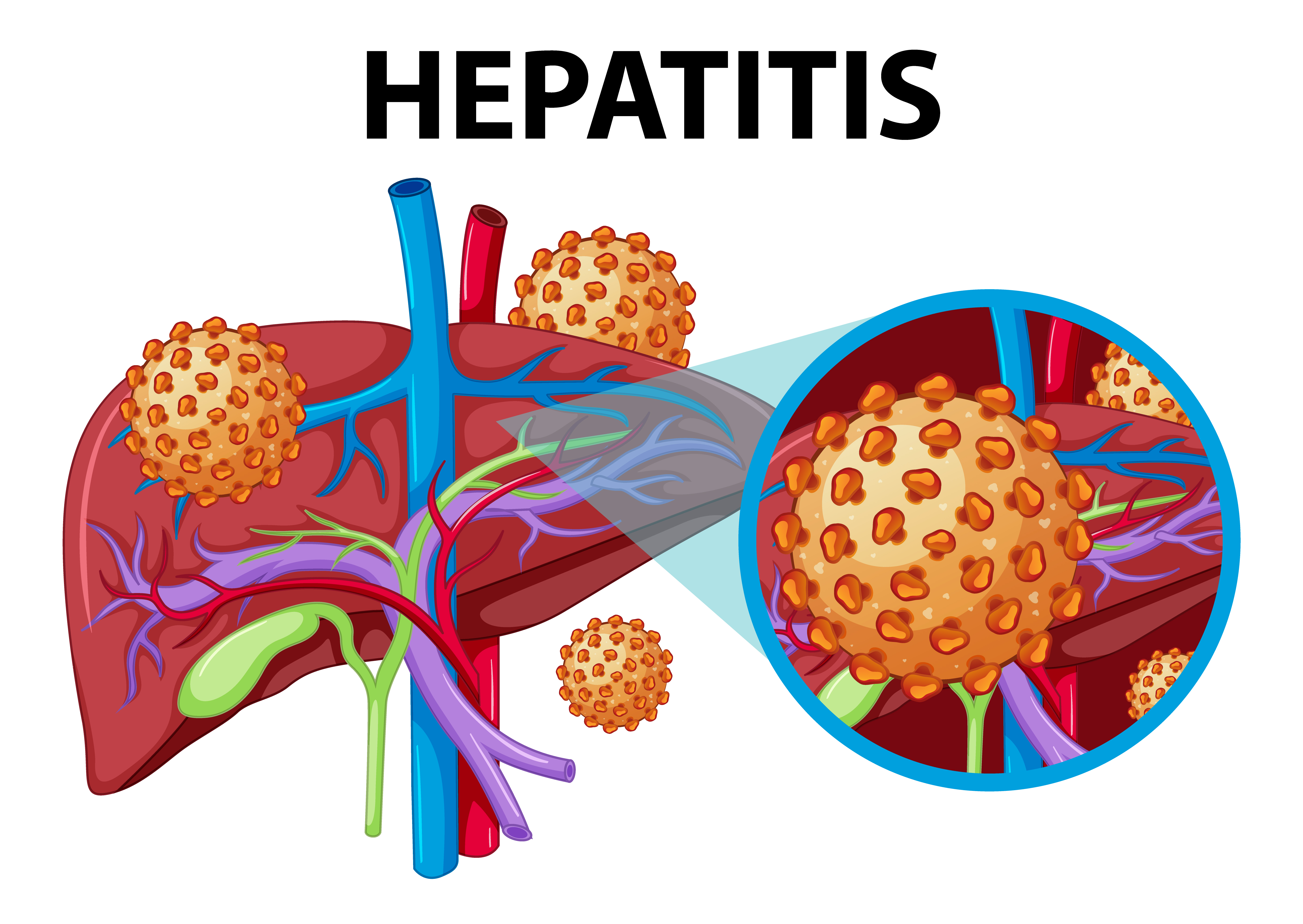
Hepatitis
Hepatitis is inflammation of the liver. Inflammation is swelling that happens when tissues of the body are injured or infected. It can damage your liver. This swelling and damage can affect how well your liver functions. Hepatitis can be an acute (short-term) infection or a chronic (long-term) infection. Some types of hepatitis cause only acute infections. Other types can cause both acute and chronic infections. The five main viral classifications of hepatitis are hepatitis A, B, C, D, and E. A different virus is responsible for each type of viral hepatitis.
Symptoms of Hepatitis
General Symptoms:
- Fatigue: Feeling unusually tired or weak.
- Abdominal Pain: Particularly in the upper right side where the liver is located.
- Loss of Appetite: Reduced desire to eat.
- Nausea and Vomiting: Feeling sick to your stomach and possibly throwing up.
- Fever: Elevated body temperature.
- Muscle and Joint Pain: Discomfort in muscles and joints.
- Dark Urine: Urine may become darker in color, sometimes described as tea-colored.
- Pale Stools: Stools may appear lighter or clay-colored.
Hepatitis-Specific Symptoms:
- Jaundice: Yellowing of the skin and the whites of the eyes, caused by a build-up of bilirubin in the blood.
- ItchySkin: Due to the accumulation of bile salts.
- Swelling: Fluid retention in the abdomen (ascites) or swelling in the legs and feet.
- EnlargedLiver or Spleen: May be felt during a physical exam.
Chronic Hepatitis Symptoms:
- Persistent Fatigue: Ongoing tiredness.
- Abdominal Discomfort: Chronic pain or discomfort in the abdominal area.
- Unexplained Weight Loss: Losing weight without trying.
- Mental Confusion: Problems with concentration or memory (hepatic encephalopathy).
Types of Hepatitis
Hepatitis A
Hepatitis A is caused by eating food and drinking water contaminated with a virus called HAV. It can also be caused by anal-oral contact during sex. While it can cause swelling and inflammation in the liver, it doesn’t lead to chronic (life-long) disease. Almost everyone who gets hepatitis A has a full recovery. There is a vaccine for hepatitis A that can be given to children or at-risk adults. Practicing good hygiene and hand washing can also reduce your risk of contracting hepatitis A virus.
Hepatitis B
Hepatitis B is caused by the virus HBV. It is spread by contact with an infected person’s blood, semen, or other body fluids. It is a sexually transmitted disease. You can get hepatitis B by:
- Having unprotected sex (not using a condom) with an infected person.
- Sharing drug needles (for illegal drugs like heroin and cocaine or legal drugs like vitamins and steroids).
- Getting a tattoo or body piercing with dirty (nonsterile) needles and tools that were used on someone else.
- Getting pricked with a needle that has infected blood on it (healthcare workers can get hepatitis B this way).
- Sharing a toothbrush, razor, or other personal items with an infected person.
- A pregnant person can give hepatitis B to the baby at birth.
- Through a bite from another person.
With hepatitis B, the liver also becomes inflamed. Hepatitis B can be a serious infection that can cause liver damage, which may result in cancer. Some people are not able to get rid of the virus, which makes the infection chronic or lifelong.
Blood banks test all donated blood for hepatitis B, greatly reducing the risk of getting the virus from blood transfusions or blood products. There is also a vaccine for hepatitis B. It is recommended for everyone, from infants to adults, to prevent contracting the disease.
Hepatitis B can be diagnosed with blood tests. The tests look for certain types of hepatitis B antigens and antibodies. These include:
- Hepatitis B surface antigen (HBsAg)
- Hepatitis B surface antibody (anti-HBs)
- Total hepatitis B core antibody (anti-HBc)
- IgM antibody to hepatitis B core antigen (IgM anti-HBc)
The hepatitis B surface antigen (HBsAg) is a protein that can be found on the surface of the HBV virus. Your immune system makes antibodies to HBsAg as a way of fighting the infection. The presence of antigens and/or antibodies can help your healthcare provider identify the phase of HBV infection and whether it is acute or chronic.
Hepatitis C
Hepatitis C is caused by the virus HCV. It can be severe and is considered to be the deadliest type of hepatitis. Hepatitis C is spread the same way as hepatitis B, through contact with an infected person’s blood or other body fluids. It can be spread via sex, but this is rare. Like hepatitis B, hepatitis C causes inflammation of the liver and can cause liver damage that can lead to cancer. If untreated, Hepatitis C can develop into a chronic infection, which can lead to liver cirrhosis. However, there are now effective treatments for HCV. Blood banks test all donated blood for hepatitis C too, significantly reducing transmission risk from transfusions and blood products. There is no vaccine for hepatitis C.
Hepatitis D
Hepatitis D is caused by the virus HDV. You can only get hepatitis D if you are already infected with hepatitis B. It is spread through contact with infected blood, dirty needles that have HDV on them, and unprotected sex (not using a condom) with a person infected with HDV. Hepatitis D causes swelling of the liver. Preventing hepatitis B by being vaccinated and avoiding blood and body fluid exposure is the best way to prevent getting hepatitis D.
Hepatitis E
Hepatitis E is caused by the virus HEV. You get hepatitis E from food or water infected with the virus. It can also be spread through oral-anal contact. It causes swelling of the liver, but usually no long-term damage. People who are pregnant or immune-compromised are at greater risk of liver damage. There is no vaccine for this virus. Practice good hygiene and avoid drinking tap water when traveling internationally.
How can we prevent Hepatitis?
- Vaccination: Vaccines are available for hepatitis A and B. Getting vaccinated can significantly reduce the risk of contracting these forms of hepatitis.
- Practicing good hygiene: Wash hands thoroughly with soap and water, especially after using the bathroom and before preparing or eating food.
- Avoiding risky behaviors: Refrain from sharing needles or engaging in unprotected sex, which can transmit hepatitis B and C.
- Ensuring safe blood transfusions: In healthcare settings, ensure that blood and other bodily fluids are handled with proper precautions to avoid transmission of hepatitis B and C.
- Practicing safe food and water habits: Avoid consuming contaminated food or water, particularly in areas where hepatitis A is prevalent.
- Maintaining a healthy lifestyle: Take precautions to prevent the transmission of hepatitis in any form, such as ensuring safe tattoo and piercing practices.
By following these measures, individuals can significantly reduce their risk of contracting hepatitis.
Who are at Risk?
Hepatitis A:
- Transmission: Typically spreads through consumption of contaminated food or water or close contact with an infected person.
- At Risk:
- Travelers to Developing Countries: Particularly those with poor sanitation.
- People with compromised immune systems: More susceptible to severe outcomes.
- Individuals in close contact with infected persons: Household or sexual contacts are at risk.
Hepatitis B:
- Transmission: Primarily through exposure to infected blood, semen, or other bodily fluids. It can also be transmitted from an infected mother to her newborn during childbirth.
- At Risk:
- Infants born to infected mothers: Without proper vaccination, newborns are at risk.
- People who inject drugs: Sharing needles or equipment increases the risk.
- Healthcare workers: Particularly those exposed to blood or body fluids.
- Sexual partners of infected individuals: Especially if unprotected sex occurs.
- People with multiple sexual partners: Increased risk of exposure.
- Individuals with chronic liver disease: More susceptible to complications.
Hepatitis C:
- Transmission: Mainly through exposure to infected blood, typically through sharing needles or other equipment used to inject drugs.
- At Risk:
- People who inject drugs: Sharing needles is a significant risk factor.
- Recipients of blood transfusions or organ transplants before 1992: When screening for hepatitis C was not as rigorous.
- Healthcare workers: Through accidental needle sticks or exposure to infected blood.
- People with HIV: Co-infection with HIV increases the risk of complications.
- Infants born to infected mothers: Less common but possible transmission during childbirth.
Hepatitis D:
- Transmission: Only occurs in individuals already infected with hepatitis B. It requires hepatitis B as a co-infection to replicate.
- At Risk:
- People with hepatitis B: Especially those who have not been vaccinated against hepatitis B.
- Injection drug users: Higher risk due to shared needles and exposure to blood.
Hepatitis E:
- Transmission: Usually through contaminated water or food, similar to hepatitis A.
- At Risk:
- Travelers to endemic areas: Where sanitation is poor.
- People with compromised immune systems: More susceptible to severe outcomes.
- Pregnant women: Particularly susceptible to severe forms of hepatitis E.
- Consumption of undercooked pork or shellfish: In areas where hepatitis E is endemic.
General Risk Factors:
- Unsafe Injection Practices: Including sharing needles or equipment for drug use or medical procedures.
- Unsafe Sexual Practices: Unprotected sex with multiple partners increases the risk of hepatitis B and, to a lesser extent, hepatitis C.
- Poor Sanitation: Particularly in developing countries where hepatitis A and E are more prevalent.
- Occupational Exposure: Healthcare workers, emergency responders, and others at risk of exposure to blood or body fluids.
- Travel to Endemic Areas: Where hepatitis A or E are prevalent due to poor sanitation or contaminated food/water sources.
Understanding these risk factors helps in both prevention efforts and early detection through screening and vaccination programs.
How hepatitis can be Diagnosed?
Hepatitis can be diagnosed through several methods, including:
- Blood Tests: The most common way to diagnose hepatitis is through blood tests that detect specific markers and antibodies related to different types of hepatitis viruses (e.g., hepatitis B surface antigen, hepatitis C antibodies).
- Liver Function Tests (LFT): These tests measure levels of enzymes and proteins that are released into the bloodstream when the liver is damaged or inflamed, which can indicate hepatitis.
- Imaging Studies: Ultrasound, CT scans, or MRI scans may be used to examine the liver and assess its condition. These can help detect signs of liver damage or abnormalities.
- Liver Biopsy: In some cases, a small sample of liver tissue may be taken for examination under a microscope to determine the extent of liver damage and to identify the specific type of hepatitis.
- Physical Examination: A healthcare provider may examine the patient for signs and symptoms of hepatitis, such as jaundice (yellowing of the skin and eyes), abdominal pain, or swelling.
- Medical History: Gathering information about risk factors, such as exposure to contaminated blood or body fluids, or travel to regions where hepatitis is endemic, can help in diagnosing the type and cause of hepatitis.
Depending on the symptoms and initial test results, healthcare providers may use one or more of these methods to accurately diagnose hepatitis and determine the appropriate treatment and management plan.
Treatment for Hepatitis
Hepatitis A:
Hepatitis A is usually a short-term illness that does not require specific treatment. Recovery is supported through:
- Rest: Adequate rest helps the body recover from the infection.
- Hydration: Drinking plenty of fluids helps prevent dehydration.
- Nutrition: A balanced diet helps support overall health.
There is no specific antiviral treatment for hepatitis A. Vaccination is an effective preventive measure.
Hepatitis B:
Treatment for hepatitis B depends on whether it is acute or chronic:
- Acute Hepatitis B: Most cases do not require specific treatment other than supportive care. However, antiviral medications may be used in severe cases or to prevent chronic infection.
- Chronic Hepatitis B: Treatment aims to suppress the virus and reduce liver damage. Antiviral medications commonly used include entecavir, tenofovir, and sometimes interferon-alpha. Regular monitoring of liver function and viral load is essential to assess the effectiveness of treatment.
Hepatitis C:
Hepatitis C can lead to chronic infection and liver damage. Treatment options have evolved significantly with the introduction of direct-acting antivirals (DAAs):
- Chronic Hepatitis C: DAAs are highly effective in curing hepatitis C. These medications target specific steps in the hepatitis C virus replication cycle. Treatment duration and specific medications depend on the genotype of the virus and individual factors.
- Monitoring: Regular monitoring during and after treatment is important to assess viral response and liver function.
Hepatitis D:
Hepatitis D is a complication of hepatitis B and is treated in conjunction with hepatitis B:
- Management of Hepatitis B: Hepatitis D requires hepatitis B to replicate. Thus, treatment focuses on managing hepatitis B with antiviral medications such as interferon-alpha, which can also suppress hepatitis D.
Hepatitis E:
Hepatitis E usually resolves on its own without specific treatment:
- Supportive Care: Similar to hepatitis A, supportive care includes rest, hydration, and proper nutrition. In cases of severe acute hepatitis E, hospitalization and supportive therapy may be necessary.
General Recommendations:
- Lifestyle Changes: Avoiding alcohol and certain medications that can harm the liver is crucial.
- Vaccination: Vaccination is available for hepatitis A and B and is recommended for prevention.
- Regular Medical Follow-Up: Monitoring liver function, viral load, and potential complications is important for all types of hepatitis, especially chronic cases.
Each type of viral hepatitis requires a tailored approach to treatment, and management should be guided by a healthcare provider familiar with liver diseases. Early diagnosis and appropriate treatment can prevent complications and improve long-term outcomes.
Hepatitis B Vaccine
It takes only a few shots to protect yourself and your loved ones against hepatitis B for a lifetime.
The hepatitis B vaccine is a safe and effective vaccine that is recommended for all infants at birth and for children up to 18 years. The hepatitis B vaccine is also recommended for adults living with diabetes and those at high risk for infection due to their jobs, lifestyle, living situations, or country of birth. Since everyone is at some risk, all adults should seriously consider getting the hepatitis B vaccine for a lifetime protection against a preventable chronic liver disease.
The hepatitis B vaccine is also known as the first “anti-cancer” vaccine because it prevents hepatitis B, the leading cause of liver cancer worldwide.














